Medical – HAP Anthem

Health coverage through Anthem offers access to an extensive network of providers for all your medical, prescription drug and mental health care needs.
Review the list of Anthem eligible expenses to see what procedures are covered, may be covered with specific documentation or are not covered.
Use the glossary of technical terms to better understand your health care plan benefits.
Using your Medical Benefits
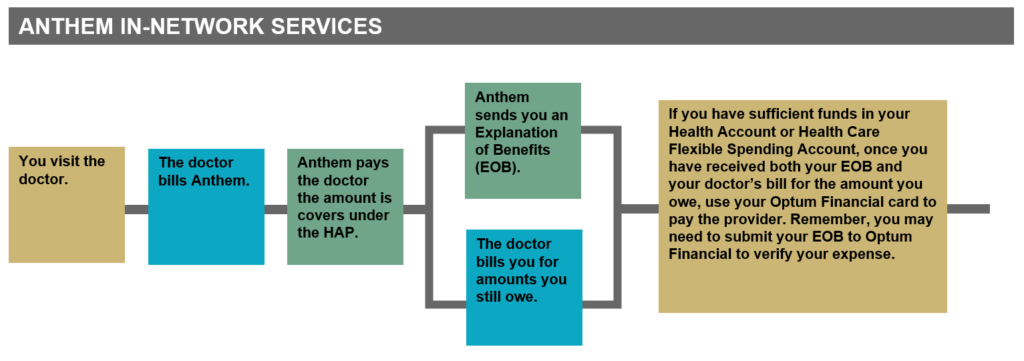
If you use an in-network provider:
You won't usually have to pay up front when you visit the doctor—but your doctor could charge you at the time of service. Your in-network doctor's office can call Anthem to find out how much you'll owe for a particular service or whether you've met your annual deductible.
Whenever you visit your in-network doctor:
- Have your Anthem ID card with you
- Know how much you have already paid toward your deductible
- Ask your doctor’s office not to charge you now and tell them you'll pay from your Health Account or Health Care Flexible Spending Account later
- Ask your doctor to call Anthem if your doctor's office wants to charge you at the time of the visit
Here's what will usually happen with an in-network doctor:
If you use an out-of-network provider:
You may have to pay the full amount at the doctor's office. Your doctor's office won't know how much you'll owe for a particular service or whether you've met the annual deductible. Your portion of the bill may be significant, so be careful. You may need to file a claim with Anthem to get reimbursed.
Prescription Drug
You can use any pharmacy. To maximize savings, use Express Scripts pharmacies and the mail-order program. You will pay the entire cost of prescriptions if you haven't met your annual deductible. Amounts paid for prescriptions apply to the annual deductible and out-of-pocket maximum. You'll never pay more in a year than your annual out-of-pocket maximum.
Some prescriptions are free
View the Anthem Retail Purchase Free Drugs List or the Express Scripts mail-order free drugs list.
Maintenance prescriptions
Most, but not all, maintenance prescriptions must use Express Scripts mail order after a maximum of three fills at a retail pharmacy.
Benefit Costs & Free Services
- Monthly Medical Rates
- View list of free services.
- View the Anthem Retail Purchase Free Drugs List or the Express Scripts mail-order free drugs list.
Telehealth & Virtual Care
With Anthem’s telehealth program, LiveHealth Online, Anthem members can use a computer or mobile device to virtually meet with a board-certified doctor, psychiatrist, or a licensed therapist from anywhere—including home and work. Learn more about LiveHealth Online Virtual Care
Health Spending Accounts
Health Account Plan (HAP)
When you enroll in medical coverage through Anthem, you automatically receive a Health Account funded by PG&E to help cover your medical expenses.
Visit the HAP-Anthem page to learn more.
Flexible Spending Accounts
In addition to the Health Account, you can also enroll in a tax-advantaged Health Care or Dependent Care Flexible Spending Account (FSA) and set aside additional funds toward necessary expenses – even if you’ve waived PG&E’s medical coverage.
The Health Care and Dependent Care FSAs are completely separate accounts. You can sign up for either or both, but you can’t transfer funds from one account to the other. See the Health Care and Dependent Care Flexible Spending Account (FSA) section below for additional details.
Visit the Spending Accounts page to learn more.
Reach out. Get help. Feel better. Contact EAP.
Contact an onsite EAP counselor, visit the EAP website, or call the EAP Hotline 24/7 at
1-888-445-4436 to speak with a licensed professional for in the moment support and to get connected to the right resource.
EAP website
Questions?
Call the PG&E Benefits Service Center at
1-866-271-8144
Monday–Friday,
7:30 am–5 pm PT
Your Health Care cards
Anthem members get three cards:
- The Anthem HAP card that tells your doctor that you’re eligible for medical benefits.
- The Express Scripts ID card tells your pharmacy you’re eligible for prescription drug benefits.
- The Optum Financial payment card will be loaded with your annual Health Account credits and – if you elected the Health Care Flexible Spending Account (FSA) – your FSA contribution.

Primary Care
You and your family members each get four free visits a year to a primary care doctor:
- General or family practitioners
- Doctors of internal medicine
- Pediatricians
- Family nurse practitioners
- OB/GYNs
- Non-hospital urgent care facilities
Did you know that you can choose and register a Personal Care Physician (PCP) with Anthem? It can make a big difference in your health. A PCP can help you stay healthy and manage certain ongoing health problems, which can help lower your health care costs and save time in getting specialized care. Click here to learn how you can find an Anthem PCP.
Specialists
You pay 20% of the cost for all specialist office visits after you meet the annual deductible. Your specialist may charge you up to the full amount of your deductible at the time of service, and you may need to file a claim to get reimbursed. You can visit any provider or specialist of your choice without preauthorization from your primary care doctor.
Urgent/Emergency Care
Urgent Care
Urgent care is covered as primary care, so you won’t have to pay a deductible. After you’ve used your four free primary care visits for the year, you pay 10% of the cost.
Some hospitals advertise themselves as urgent care centers when in fact, they’re not and they charge higher emergency room rates. This can make a big difference in how much you pay out of your own pocket.
Always check to see if the facility you want to use is really an urgent care center.
Go to anthem.com/ca/pge or access the Anthem BlueCross smartphone app to find an urgent care center near you.
Emergency Care
You pay 20% of the cost, subject to the annual deductible. After you visit the emergency room, your HAP plan administrator—Anthem—will process the claim and then send you an Explanation of Benefits (EOB).
Mental Health & Substance Use Disorder Care
Carelon Behavioral Health administers all mental health and substance use disorder care for Anthem.
Here’s what you pay for services:
- Outpatient services: You pay 10% of the cost with no deductible
- Inpatient services: You pay 20% of the cost after you meet the annual deductible
To preauthorize care, contact:
- A Carelon care manager 24/7 at 1-888-445-4436
- An onsite Employee Assistance Program (EAP) counselor during normal business hours
Finding a Counselor or Psychiatrist
It’s important to find someone who is trained to treat your problem, makes you feel comfortable, and is someone you can trust. Click here for helpful hints on finding someone who is a good fit for you.
- Schedule a telehealth appointment with an in-network psychiatrist or licensed therapist via chat, text, audio, or video (please see the Telehealth & Virtual Physical and Mental Health Care tab).
- Call 1-888-445-4436 for assistance selecting an in-network provider. If the referrals don’t work out, call back and request a Provider Search—the staff will conduct an outreach to find providers that are available. Share the names of the providers who were full or didn’t call back so Carelon can update their directory.
- Find a list of in-network providers on Carelon’s online tool.
- Seek an out-of-network provider, request a superbill, and submit the claim for reimbursement (see File a Claim below). You’ll pay balance billing in addition to 10% co-insurance.
Benefit of Using In-Network Providers
You generally will be charged fees that are higher than the NEGOTIATED RATE charged by a NETWORK PROVIDER and will be responsible for the portion of those fees that are over the allowed amount. You may also be responsible for any ineligible expenses or even the entire bill. You should discuss this with your PROVIDER, as these amounts can be substantial. Read more here.
File a Claim
To file a claim for reimbursement, log on to the Carelon website > Manage Benefits. If you’re creating an account for the first time, enter your social security number where a nine-digit member ID number is requested.
Substance Use Disorder Treatment
There are a range of formal treatment options for substance use disorders such as detoxification, acute inpatient treatment, intensive outpatient treatment and residential treatment which require meeting medical necessity in order to be covered by your health insurance plan. There are also 12-step programs, such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), which anyone can attend. With the guidance of a skilled care manager, you can determine which type of treatment would be most effective and appropriate for you. Call 1-888-445-4436 to get the process started.
Telehealth Alcohol Treatment Program: Covered by Carelon for Anthem members, Ria Health is an innovative telehealth alcohol treatment program that uses medications, online counseling, and support to help you achieve lasting results.
- Expert physician guidance, care, support, and customized treatment plans.
- Medications that reduce alcohol cravings, helping people quit or drink less.
- Withdrawal management.
- Weekly telehealth meetings with a certified recovery coach.
- Bluetooth-enabled breathalyzer and smartphone app to track progress.
- Regular online group support meetings facilitated by a recovery coach.
Get started by calling Ria Health at 877-343-5131 or online at riahealth.com/lp/pge.
Telehealth options
If you’d like to see a counselor or psychiatrist via telehealth, please see the Telehealth & Virtual Physical and Mental Health Care tab above.
Telehealth Alcohol Treatment Program: Covered by Carelon for Anthem members, Ria Health is an innovative telehealth alcohol treatment program that uses medications, online counseling, and support to help you achieve lasting results.
- Expert physician guidance, care, support, and customized treatment plans.
- Medications that reduce alcohol cravings, helping people quit or drink less.
- Withdrawal management.
- Weekly telehealth meetings with a certified recovery coach.
- Bluetooth-enabled breathalyzer and smartphone app to track progress.
- Regular online group support meetings facilitated by a recovery coach.
Get started by calling Ria Health at 877-343-5131 or online at riahealth.com/lp/pge.
Autism and Applied Behavior Analysis (ABA)
Applied Behavior Analysis services are also provided through Carelon (at no charge, with no deductible). To obtain prior authorization or pre-certification, please call 1-888-445-4436. During this call, a care manager will request basic information — including, but not limited to — a child’s diagnosis, who made the diagnosis, and what the presenting symptoms are (e.g., developmentally delayed skills, problem behaviors). Click here to learn more. (Must be connected to PG&E network to view.)
Cancer resources
If you or your loved one has been touched by cancer, you may have questions and need to make some timely decisions. To help you during this time, PG&E provides you and your covered dependents with Anthem’s case management program — a cancer resource that specializes in oncology, and is designed to help members understand what to expect and plan how to move forward with a cancer diagnosis.
A nurse specially trained to support oncology patients will be available by phone to:
- Answer your questions
- Explain next steps
- Connect you with resources to support you
- Enroll you in outreach support from the American Cancer Society if you choose
Are you currently undergoing treatment for cancer? If you have questions about benefits or resources, please contact Anthem for referral to a case manager: 1-888-613-1130. Representatives are available Monday through Friday from 9 a.m. to 8 p.m. and Saturday 9 a.m. to 4:30 p.m. Pacific time.
No matter where you are in life, we’re making it easier for you to receive the high-quality care you need.
Benefits while traveling
If you’re traveling or living outside of your home state, you can use Anthem’s BlueCard Program to access a broader network of doctors and hospitals at discounted rates through other Blue Cross/Blue Shield plans. To locate BlueCard PPO providers:
- Call Anthem Blue Cross Member Services at 1-800-810-2583 (the number is printed on the back of your Anthem ID card for easy reference)
- Visit www.anthem.com/ca/pge
You’ll be able to visit any provider or specialist of your choice without preauthorization from your primary care doctor.
Benefits for family members living away from home
Dependents who live away from home — like college students — can use Anthem’s BlueCard Program to access a broader network of doctors and hospitals at discounted rates through other Blue Cross/Blue Shield plans. To locate BlueCard providers:
- Call Anthem Blue Cross Member Services at 1-800-810-2583 (the number is printed on the back of your Anthem ID card for easy reference)
- Visit www.anthem.com/ca/pge
Filling a prescription at the pharmacy
You can use any pharmacy for prescriptions, but you’ll have lower costs when you use an Anthem in-network Express Scripts pharmacy.
At an in-network Express Scripts pharmacy, the pharmacist can tell you exactly how much you owe for a particular drug. You can use your Optum Financial payment card to pay for prescriptions and some over-the-counter health care supplies. If you don’t have enough in your Health Account (and Health Care Flexible Spending Account (FSA), if you’ve elected it), you’ll need to pay out-of-pocket. You can also go to express-scripts.com to view your statement.
At an out-of-network pharmacy, you can use your Optum Financial payment card to pay for the entire cost of the prescription. However, not all small, independent pharmacies have the correct computer system to validate your transaction, in which case you’ll need to pay for the prescription using another form of payment. In all instances, if you pay 100% up front, you will then have to file a claim with Express Scripts for reimbursement. To file a claim, complete the Express Scripts Prescription Reimbursement / Coordination of Benefits Form. The form can also be obtained by calling Express Scripts at 1-800-718-6590 or by downloading it at express-scripts.com.
Want to manage your prescriptions on the go? Use the express scripts app to request refills and renewals, track mail-order prescriptions, get alerts about possible drug interactions and more.
Filling a prescription for maintenance medications
You must use the Express Scripts mail-order program for certain maintenance medications. You can get up to three fills of the same prescription from a retail pharmacy before you have to switch to mail order. If you don’t switch to mail order after three fills, you’ll have to pay 100% of the cost at the pharmacy — and this does not apply to your deductible or out-of-pocket maximum.
Most narcotics, ADHD drugs, and compound drugs are not part of the mandatory mail-order requirement; you’ll need to purchase these at a retail pharmacy.
Filling a prescription by mail
You can get up to a 90-day supply of medication for each prescription when you use the Express Scripts mail-order program. You must use the Express Scripts mail-order program for certain maintenance medications. You can get up to three fills of the same prescription from a retail pharmacy before you have to switch to mail order. If you don’t switch to mail order for those maintenance medications, you’ll pay 100% of the cost and nothing will apply to your deductible or out-of-pocket maximum.
The first time you order, you’ll need to complete two Express Scripts forms:
- Mail-order form
- Health, Allergy and Medication Questionnaire (HMQ), which alerts the pharmacists who are filling your mail-order prescriptions of any allergies or medical conditions that might be affected by the prescriptions you’re ordering
You’ll need to mail the completed forms with your original prescription to:
Express Scripts
P.O. Box 747000
Cincinnati, Ohio 45274-7000
To get the Express Scripts mail-order form, Health Assessment Questionnaire, and mail-order envelopes:
- Call Express Scripts Member Services at 1-800-718-6590
- Download them from the Express Scripts website
Filling a prescription for an opioid
If your doctor or dentist prescribes you an opioid, here’s what you should know.(Must be connected to PG&E network to view.)
Doctor Visits
Easily accessible and convenient 24/7, LiveHealth Online saves you time and the hassle of driving to a doctor’s office for consultation when you’re sick, have a rash or even to receive a prescription. There are no appointments or long lines to see a doctor, and it’s already part of the Anthem Health Account Plan (HAP).
The cost for a virtual doctor appointment is only $5.90, if you are an Anthem HAP member. If you aren’t enrolled in the Anthem HAP, the cost is $59. You can use your Health Account to pay this cost.
Register to get started.
Mental Health Visits
Visit a licensed therapist.
- LiveHealth Online: Have a video visit with a therapist to get help with anxiety, depression, grief, panic attacks and more. Schedule your psychology appointment online (see below) or call
1-888-548-3432 from 8 a.m. to 8 p.m., seven days a week. You’ll see the cost before the visit starts and you pay just a 10% co-insurance, no deductible. To schedule a video visit for a child, ages 10 and up, just log in to your account and choose LiveHealth Online Psychology for Teens. Register to get started. - Talkspace: Through Carelon’s Talkspace program, Anthem members ages 13 and older can get matched with a therapist for support via text, chat, phone and/or video call.
Consult a board-certified psychiatrist
- LiveHealth Online: If you’re over 18 years old, you can get medication support to help you manage a mental health condition. Schedule your appointment online (see below) or call
1-888-548-3432 from 8 a.m. to 8 p.m., seven days a week. You’ll see the cost before the visit starts and you pay just a 10% co-insurance, no deductible. Your Anthem plan includes benefits for video visits using LiveHealth Online, so you’ll just pay your share of the costs. Register to get started. - Talkspace: Through Carelon’s Talkspace program, Anthem members ages 18 and older can schedule a video appointment with a psychiatrist.
Remember, if you’re in crisis or having suicidal thoughts, go to the nearest emergency room or call 911.
Alcohol Treatment via Telehealth
Available for Anthem members via Carelon Behavioral Health, Ria Health is an innovative telehealth alcohol treatment program that uses medications, online counseling, and support to help you achieve lasting results.
- Expert physician guidance, care, support, and customized treatment plans.
- Medications that reduce alcohol cravings, helping people quit or drink less.
- Withdrawal management.
- Weekly telehealth meetings with a certified recovery coach.
- Bluetooth-enabled breathalyzer and smartphone app to track progress.
- Regular online group support meetings facilitated by a recovery coach.
Get started by calling Ria Health at 877-343-5131 or online at riahealth.com/lp/pge/.
Sleep Specialist Visits
Visit with a board-certified sleep specialist.
Visit with a board-certified sleep specialist for an initial evaluation, referral for testing if appropriate, a personalized treatment plan, and follow-up visits as needed for a wide range of sleep disorders. Register to get started.
Get Started
LiveHealth Online
Register by going to livehealthonline.com or downloading the Live HealthOnline iPhone or Android apps. When accessing the service at a PG&E worksite, you must use cell service to connect. Virtual visits cannot be accessed through PG&E’s Wi-Fi.
For additional information about Anthem’s telehealth program, please refer to the LiveHealth Online FAQs, email customersupport@livehealthonline.com or call 1-855-603-7985.
As a reminder, if you have a work-related discomfort or injury, call the 24/7 Nurse Care Line at
1-888-449-7787.
Talkspace
Register by going to talkspace.com/carelonbehavioralhealth and entering the primary subscriber’s eight-digit PG&E personnel number (PRNR) when the Talkspace website prompts for the member/subscriber ID. Once you create an account, you can connect with a provider using the Talkspace app or your computer.
For additional information about the Talkspace program, call Carelon at 1-888-445-4436.
Ria Health
Get started with telehealth alcohol use disorder treatment by calling Ria Health at 1-877-343-5131 or online at riahealth.com/lp/pge. Call Carelon at 1-888-445-4436 for additional information.
